Health Insurance Coverage for Autism
Unlocking health insurance coverage for autism care. Discover the types of plans, therapy coverage, and how to advocate for better benefits.


Understanding Health Insurance Coverage for Autism
When it comes to providing comprehensive care for individuals with autism, health insurance plays a vital role. Understanding the importance of health insurance coverage for autism care and the different types of health insurance plans available is crucial for families seeking the best support for their loved ones.
Importance of Health Insurance for Autism Care
Health insurance coverage is essential for individuals with autism as it helps to offset the significant costs associated with diagnosis, therapy, and ongoing treatment. Autism spectrum disorder (ASD) requires a multidisciplinary approach, involving various healthcare professionals and specialized services. Without adequate insurance coverage, the financial burden of these services can be overwhelming for families.
Health insurance coverage for autism typically includes benefits for diagnostic assessments, behavioral therapy, occupational therapy, speech therapy, and other essential services. By providing access to these services, health insurance plays a crucial role in improving the quality of life for individuals with autism and supporting their overall development.
Types of Health Insurance Plans
There are different types of health insurance plans available that provide coverage for autism care. Some common types include:
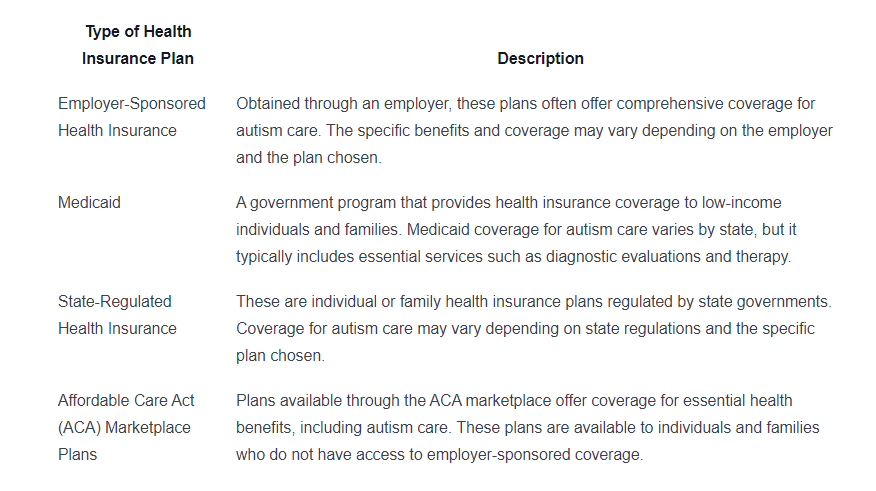
It is important for individuals and families to carefully review and compare the benefits and coverage offered by different health insurance plans. Understanding the specific details of each plan, such as deductibles, co-payments, and coverage limits, can help determine which plan provides the most comprehensive coverage for autism care.
By understanding the importance of health insurance coverage for autism care and exploring the different types of health insurance plans available, individuals and families can make informed decisions to ensure access to the necessary services and support for individuals with autism.

Coverage for Autism Services
When it comes to health insurance coverage for autism, it's essential to understand the specific services that are typically covered. Insurance plans vary in terms of the services they include, so it's important to familiarize yourself with the coverage options available to ensure access to the necessary care. In this section, we will explore the coverage for behavioral therapy, occupational therapy, and speech therapy.
Behavioral Therapy Coverage
Behavioral therapy is a fundamental component of autism treatment, focusing on improving behavior, communication, and social skills. Many insurance plans recognize the importance of behavioral therapy and provide coverage for it. However, the extent of coverage may vary.
Before seeking behavioral therapy, it's crucial to review your insurance plan to determine the coverage details. Some plans may have specific requirements, such as pre-authorization or a referral from a healthcare provider. Additionally, coverage limits and the number of sessions allowed per year may also be specified.
Occupational Therapy Coverage
Occupational therapy aims to enhance an individual's ability to perform daily activities and develop skills for independent living. This type of therapy can be beneficial for individuals with autism, who may experience challenges in areas such as motor skills, sensory processing, and self-care.
Insurance plans often provide coverage for occupational therapy services, but it's important to understand the specific terms and conditions. This includes checking whether the therapy must be provided by an in-network provider, any pre-authorization requirements, and any coverage limitations or exclusions.
Speech Therapy Coverage
Speech therapy focuses on improving communication skills, including speech, language, and social interaction. For individuals with autism, speech therapy can play a vital role in developing effective communication strategies.
Insurance plans commonly include coverage for speech therapy services. However, it's important to review the details of your specific plan. This includes determining whether the therapy must be provided by an in-network provider, any requirements for pre-authorization, and any coverage limitations or exclusions.
To gain a better understanding of the coverage for autism services, it's recommended to review the policy documents and contact the insurance provider directly. They can provide specific information regarding coverage, including any paperwork or documentation required for reimbursement.
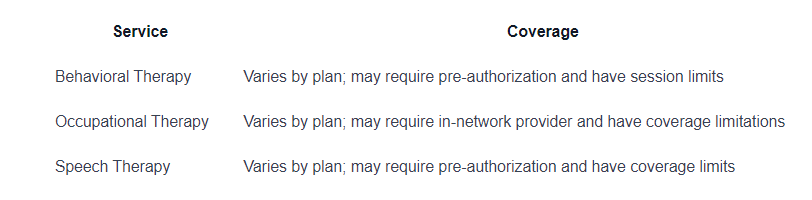
By being informed about the coverage for behavioral therapy, occupational therapy, and speech therapy, individuals and families can better navigate the insurance system and access the necessary services for autism care.
Evaluating Insurance Plans
When it comes to health insurance coverage for autism, it's essential to carefully evaluate the different insurance plans available. Understanding the key factors to consider can help you make an informed decision regarding the coverage that best suits your needs. Here are three important aspects to evaluate when assessing insurance plans for autism:
In-Network vs. Out-of-Network Providers
Insurance plans often have a network of preferred providers, including doctors, therapists, and specialists. These providers are considered in-network, meaning they have established contracts with the insurance company. In-network providers typically have negotiated rates and agreed-upon coverage for specific services.
Using in-network providers can be advantageous as it often results in lower out-of-pocket costs for the policyholder. Utilizing out-of-network providers, on the other hand, may lead to higher costs, as the insurance company may cover a smaller percentage of the expenses or require higher deductibles.
When evaluating insurance plans for autism, it's important to check whether your preferred healthcare providers are in-network. This ensures that you can access the necessary services while minimizing your financial burden.
Prior Authorization Requirements
Some insurance plans require prior authorization for specific treatments or services. Prior authorization is the process of obtaining approval from the insurance company before receiving the recommended treatment. This is done to ensure that the treatment is medically necessary and appropriate.
When considering insurance plans for autism, it's crucial to understand the prior authorization requirements. Familiarize yourself with the procedures and documentation needed to obtain prior authorization for services such as behavioral therapy, occupational therapy, or speech therapy. Being aware of these requirements can help prevent unexpected denials and delays in receiving crucial services.
Coverage Limits and Exclusions
Insurance plans often have coverage limits and exclusions that affect the extent of coverage for autism-related services. Coverage limits refer to the maximum amount the insurance company will pay for a particular service or treatment. Exclusions, on the other hand, are specific services or treatments that the insurance plan does not cover.
When evaluating insurance plans for autism, it's important to review the coverage limits and exclusions related to behavioral therapy, occupational therapy, and speech therapy. Understanding these limitations can help you determine the level of coverage provided and whether it meets your specific needs.
Here's an overview of coverage limits for common autism services:
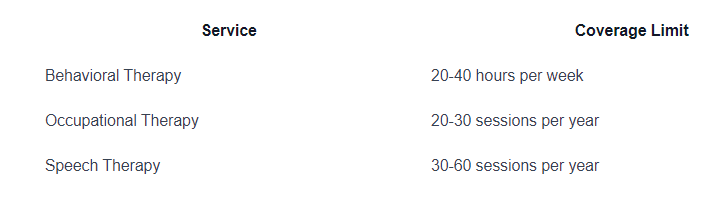
Remember to carefully review the coverage limits and exclusions in the insurance plan's policy documents to ensure you have a clear understanding of what is covered and what is not.
By thoroughly evaluating insurance plans for autism, considering factors such as in-network providers, prior authorization requirements, and coverage limits and exclusions, you can make an informed decision that aligns with your specific needs and helps provide the necessary support for individuals with autism.

Utilizing Health Insurance Benefits
When it comes to obtaining the necessary care for autism, understanding how to utilize your health insurance benefits is essential. This section will focus on two important aspects: submitting claims and understanding co-payments and deductibles.
Submitting Claims
To ensure that you receive the appropriate reimbursement for autism-related services, it is crucial to understand the process of submitting claims to your health insurance provider. Here are the general steps involved in submitting a claim:
- Obtain the necessary documentation: Collect all relevant invoices, receipts, and treatment documentation from your healthcare provider. This includes details such as the date of service, type of service provided, and the provider's information.
- Complete the claim form: Fill out the claim form provided by your health insurance company. This form typically requires information such as your personal details, policy number, and the details of the services received.
- Attach supporting documents: Include all the necessary supporting documents, such as invoices and receipts, along with the completed claim form. Make sure to keep copies of these documents for your records.
- Submit the claim: Send the completed claim form and supporting documents to your health insurance provider. Follow their preferred method of submission, which is often through mail or online portals.
- Follow up on the claim: Keep track of your claim's progress by regularly checking with your health insurance provider. This will help ensure that your claim is being processed and that any necessary additional information is provided promptly.
Understanding the process of submitting claims can help streamline the reimbursement process and ensure that you receive the maximum coverage for your autism-related services.
Understanding Co-Payments and Deductibles
Co-payments and deductibles are important terms to be familiar with when utilizing your health insurance benefits for autism care.
- Co-payments: A co-payment, or co-pay, is a fixed amount that you are required to pay out-of-pocket for each visit or service. This amount is predetermined by your health insurance plan and may vary depending on the type of service received.
- Deductibles: A deductible is the amount you must pay out-of-pocket before your health insurance coverage begins to contribute. For example, if your deductible is $500, you will be responsible for paying the first $500 of covered services before your insurance starts covering a portion of the costs.
It's important to review your health insurance plan to understand the specific co-payment and deductible amounts applicable to autism services. Keep in mind that these amounts can vary depending on the plan and the specific services received.
By understanding the process of submitting claims and the role of co-payments and deductibles, you can effectively navigate your health insurance benefits for autism care. This knowledge empowers you to make informed decisions, optimize your coverage, and access the necessary services and support for individuals with autism.
Advocating for Better Coverage
When it comes to health insurance coverage for autism, it's important for individuals and families to advocate for better coverage options. By seeking coverage improvements and utilizing available resources and support groups, you can play an active role in promoting better access to essential autism services.
Seeking Coverage Improvements
Advocating for better coverage starts with understanding the current gaps and limitations in insurance plans. By identifying areas where coverage falls short, you can work towards improving the benefits and services available for individuals with autism. Here are a few steps you can take to seek coverage improvements:
- Research and stay informed: Stay up-to-date with the latest policies and regulations related to health insurance coverage for autism. Understand the existing laws and guidelines in your region that protect the rights of individuals with autism and their families.
- Engage with advocacy organizations: Join local or national advocacy organizations that focus on autism and healthcare. These organizations often work towards improving insurance coverage and can provide valuable resources and guidance on advocating for better policies.
- Contact legislators and policymakers: Reach out to your elected representatives and policymakers to voice your concerns about the current state of health insurance coverage for autism. Write letters, make phone calls, or attend community meetings to express the need for better access to necessary services.
- Participate in public forums and discussions: Attend public forums, town hall meetings, or public hearings related to health insurance and autism. Share your experiences and challenges faced in obtaining appropriate coverage, and highlight the importance of comprehensive coverage for autism services.
- Collaborate with other advocacy groups: Partner with other advocacy groups, such as disability rights organizations or mental health associations, to amplify your efforts. Working together with like-minded organizations can help create a stronger collective voice for change.
Utilizing Resources and Support Groups
In addition to seeking coverage improvements, it's essential to utilize available resources and support groups to navigate the complexities of health insurance coverage for autism. These resources can provide valuable information and guidance, ensuring that you make the most of your insurance benefits. Here are some ways to utilize these resources:
- Insurance company resources: Contact your insurance provider directly to understand the specific coverage options available for autism services. They can provide you with policy documents, coverage details, and information on how to access necessary services.
- Autism advocacy organizations: Connect with autism advocacy organizations that offer resources and support specifically related to health insurance coverage. These organizations often provide educational materials, webinars, and workshops to help individuals and families navigate the insurance system.
- Local support groups: Join local support groups or online communities where you can connect with other individuals and families facing similar challenges. These groups can provide valuable insights and firsthand experiences about navigating health insurance coverage for autism in your specific region.
- Insurance case managers: If available, seek assistance from insurance case managers who specialize in autism services. These professionals can guide you through the insurance process, help you understand coverage options, and provide support in advocating for necessary services.
By actively advocating for better coverage and utilizing available resources, you can contribute to improving access to essential autism services. Remember, change may take time, but your efforts can make a difference in ensuring that individuals with autism receive the support and care they need.
Sources
https://www.autismspeaks.org/health-insurance
https://www.abtaba.com/blog/health-insurance-coverage-for-autism
https://www.insurance.ca.gov/01-consumers/110-health/60-resources/05-autism/
Similar articles
We’re here to help you

Our team is here to assist you in this process. Contact us for any assistance.
it’s easy to apply
We Accept Most Insurances
Our in-network insurance partnerships make ABA therapy more accessible to families throughout our service areas.







Our Insurance Process
We'll request your insurance details to help us verify your plan's coverage for ABA therapy. Once we've received this information, we'll walk you through your benefits, including copayments, deductibles and out-of-pocket maximums, so you know what to expect in advance.
Our team will then handle the preauthorization and all the necessary paperwork.
.svg)


















.jpeg)


























.jpeg)




.jpeg)







.jpeg)










.jpeg)