Childhood Disintegrative Disorder
Discover childhood disintegrative disorder: symptoms, causes, diagnosis, treatment, and long-term support options. Find hope and healing.

Understanding Childhood Disintegrative Disorder
Childhood Disintegrative Disorder (CDD) is a rare developmental disorder that affects children. It is characterized by a significant regression in multiple areas of functioning after a period of normal development. Let's explore what CDD entails and the symptoms that help in its diagnosis.

What is Childhood Disintegrative Disorder (CDD)?
Childhood Disintegrative Disorder, also known as Heller's syndrome, is a neurological condition that typically emerges in early childhood. Children with CDD experience a severe loss of previously acquired skills in multiple domains, such as language, social interaction, motor skills, and self-care abilities.
The onset of CDD usually occurs between the ages of 2 and 4 years, and the regression is often rapid and extensive. The condition is much rarer than other pervasive developmental disorders, such as Autism Spectrum Disorder (ASD).
Symptoms and Diagnostic Criteria of CDD
To diagnose Childhood Disintegrative Disorder, healthcare professionals rely on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). These criteria include:
- Significant loss of previously acquired skills: Children with CDD experience a substantial decline in language, social, motor, and self-care skills.
- Regression in multiple areas: The regression must occur in at least two of the following areas: expressive or receptive language, social skills or adaptive behavior, bowel or bladder control, play, or motor skills.
- Age of onset: The symptoms must emerge after a period of at least two years of relatively normal development.
- Absence of other medical or neurological conditions: The regression cannot be better explained by another medical or neurological condition.
It's important to note that the symptoms of CDD can vary widely among affected individuals. Some children may exhibit additional behavioral issues, sensory abnormalities, or cognitive impairments. A comprehensive evaluation by a qualified healthcare professional is crucial to differentiate CDD from other developmental disorders.
Understanding the fundamentals of Childhood Disintegrative Disorder sets the stage for exploring its causes, risk factors, diagnosis, treatment, and long-term outlook. By recognizing the unique challenges faced by children with CDD, we can work towards providing the necessary support and intervention for their well-being and development.
Causes and Risk Factors
Childhood Disintegrative Disorder (CDD) is a complex neurodevelopmental disorder with various potential causes and risk factors. Understanding these factors can contribute to a better understanding of the disorder and its management.
Potential Causes of CDD
The exact cause of Childhood Disintegrative Disorder is not yet fully understood. However, researchers have identified several potential factors that may contribute to the development of CDD. These include:
- Genetic Factors: Studies have suggested a potential genetic component in the development of CDD. Certain gene mutations or variations may predispose individuals to the disorder. However, more research is needed to establish a definitive link.
- Neurological Abnormalities: Brain abnormalities or disruptions in brain development have been observed in individuals with CDD. These abnormalities may affect the areas of the brain responsible for language, social interaction, and other developmental skills.
- Environmental Factors: Some environmental factors, such as prenatal and perinatal complications, exposure to toxins, or infections during critical periods of development, have been proposed as potential contributors to CDD. However, the specific environmental triggers are not yet clearly identified.
- Immunological Factors: Alterations in the immune system functioning have also been suggested as a possible cause of CDD. Abnormal immune responses or autoimmune reactions may play a role in the development or progression of the disorder.
Risk Factors Associated with CDD
Certain factors may increase the risk of a child developing Childhood Disintegrative Disorder. These risk factors include:
- Gender: CDD is more commonly diagnosed in boys than in girls. The reason for this gender disparity is not fully understood.
- Age: CDD typically manifests between the ages of 2 and 4 years, after a period of normal development. The regression in skills and the onset of symptoms during this critical age range are characteristic of the disorder.
- Family History: Having a family history of neurodevelopmental disorders, including autism spectrum disorder (ASD), may increase the risk of a child developing CDD. This suggests a potential genetic predisposition.
- Environmental Factors: Exposure to certain environmental factors, such as maternal infections during pregnancy or complications during birth, may increase the risk of CDD. However, more research is needed to understand the specific environmental factors involved.
Understanding the potential causes and risk factors associated with Childhood Disintegrative Disorder can aid in early identification, intervention, and treatment. It is important to note that these factors are not definitive predictors, and each child's experience with CDD may vary. Further research is needed to gain a deeper understanding of the complex interplay between these factors and the development of CDD.
Diagnosis and Treatment
When it comes to childhood disintegrative disorder (CDD), an early and accurate diagnosis is crucial for effective management. In this section, we will delve into the diagnostic process for CDD and explore the treatment approaches available for managing this condition.
Diagnostic Process for CDD
Diagnosing childhood disintegrative disorder involves a comprehensive evaluation by healthcare professionals, including pediatricians, child psychiatrists, and developmental specialists. The diagnostic process typically includes the following steps:
- Medical History and Physical Examination: The healthcare provider will gather a detailed medical history, including information about the child's developmental milestones and any regression observed. A physical examination may also be conducted to rule out any underlying medical conditions.
- Assessment of Developmental Skills: The child's developmental skills and abilities will be assessed using standardized tests, such as the Autism Diagnostic Observation Schedule (ADOS) and the Childhood Autism Rating Scale (CARS). These assessments help to identify any significant delays or regression across multiple domains, such as language, social interaction, and motor skills.
- Diagnostic Criteria: The healthcare provider will compare the child's symptoms and developmental regression against the diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Meeting the specific criteria for CDD is essential for an accurate diagnosis.
- Additional Evaluations: In some cases, additional evaluations may be recommended to rule out other conditions that may present with similar symptoms. These evaluations may include genetic testing, brain imaging, or specialized assessments by speech and language pathologists or occupational therapists.
Once a diagnosis of childhood disintegrative disorder is confirmed, a comprehensive treatment plan can be developed to address the unique needs of the child.
Treatment Approaches for Managing CDD
There is currently no cure for childhood disintegrative disorder, but early intervention and a multidisciplinary approach can help manage the symptoms and improve the child's quality of life. The treatment approaches for managing CDD may include:
- Behavioral and Educational Interventions: Applied Behavior Analysis (ABA), structured teaching methods, and individualized educational programs can help children with CDD develop essential skills, improve communication, and enhance social interactions.
- Speech and Language Therapy: Speech and language therapy can assist children with CDD in developing and improving their communication skills. Therapists may use various techniques, such as augmentative and alternative communication (AAC), to facilitate effective communication.
- Occupational Therapy: Occupational therapy focuses on enhancing the child's fine motor skills, self-care abilities, and sensory integration. Occupational therapists may provide interventions to improve daily living skills and promote independence.
- Medications: In some cases, medications may be prescribed to manage specific symptoms associated with CDD, such as hyperactivity, aggression, or sleep disturbances. The use of medications is determined on an individual basis and should be closely monitored by healthcare professionals.
- Family Support and Counseling: Providing emotional support and counseling to the family is crucial in managing CDD. Families may benefit from joining support groups, accessing counseling services, and receiving guidance on coping strategies and resources.
It's important to note that the treatment plan for managing childhood disintegrative disorder should be individualized based on the child's unique needs and strengths. Regular monitoring and adjustments to the treatment approach may be necessary to ensure the child receives the optimal support and care.
By diagnosing CDD early and implementing appropriate interventions, healthcare professionals and families can work together to support children with CDD and promote their overall well-being and development.
Supporting a Child with CDD
Childhood Disintegrative Disorder (CDD) can significantly impact the lives of both the affected child and their family. Providing a supportive environment and using effective strategies for communication and interaction are essential in helping a child with CDD reach their full potential.
Creating a Supportive Environment
Creating a supportive environment for a child with CDD involves a combination of understanding their unique needs and implementing strategies to meet those needs. Here are some key considerations:
- Structure and Routine: Establishing a structured daily routine can provide a sense of predictability and security for the child. Consistency in daily activities, such as meals, playtime, and bedtime, can help them feel more comfortable and reduce anxiety.
- Visual Supports: Visual supports, such as schedules, charts, and visual cues, can assist in communication and understanding. Using visual aids can help the child anticipate and navigate daily activities, transitions, and expectations.
- Sensory-Friendly Environment: Children with CDD may have sensory sensitivities. Creating a sensory-friendly environment involves minimizing unnecessary sensory stimuli, providing sensory outlets, and ensuring a calm and safe space for the child.
- Positive Reinforcement: Encouragement and positive reinforcement play a crucial role in supporting a child with CDD. Acknowledge their efforts and achievements, no matter how small, to promote self-esteem and motivation.
- Collaboration and Support: Seek support from professionals, such as therapists, educators, and support groups specializing in CDD. Collaborating with these individuals can provide valuable insights, guidance, and resources to support the child's development.
Strategies for Communication and Interaction
Effective communication and interaction strategies can help bridge the gap between a child with CDD and their caregivers, peers, and educators. Here are some strategies to consider:
- Visual Communication: Utilize visual supports, such as picture cards, symbol boards, or sign language, to enhance communication. Visual cues can assist the child in expressing their needs, wants, and emotions.
- Simplified Language: Use clear, concise, and simple language when communicating with the child. Break instructions or information into smaller, manageable parts to facilitate understanding.
- Social Stories: Social stories are short narratives that describe specific situations, social cues, and expected behaviors. Using social stories can help the child understand social situations and appropriate responses.
- Nonverbal Communication: Nonverbal cues, such as facial expressions, gestures, and body language, play a significant role in communication. Pay attention to the child's nonverbal cues and respond accordingly.
- Structured Play and Social Skills Training: Engage the child in structured play activities and social skills training to facilitate social interaction and development. These activities can focus on turn-taking, sharing, and understanding emotions.
Supporting a child with CDD requires patience, understanding, and a willingness to adapt strategies to meet their individual needs. Remember, each child is unique, and what works for one may not work for another. By creating a supportive environment and implementing effective communication and interaction strategies, you can help the child thrive and reach their full potential.
Prognosis and Long-Term Outlook
Childhood Disintegrative Disorder (CDD) is a rare condition that can have a significant impact on a child's development and overall functioning. Understanding the prognosis and long-term outlook for children diagnosed with CDD is essential for parents, caregivers, and healthcare professionals involved in their care.
Prognosis of Children with CDD
The prognosis of children with CDD varies depending on the severity of the condition and individual factors. Unfortunately, CDD is associated with a generally poor prognosis. Most children with CDD experience a significant loss of skills and functioning, which can affect their ability to communicate, socialize, and perform everyday tasks.
The onset of CDD typically occurs between the ages of 2 and 4 years, and regression in multiple areas of development is a hallmark feature of the disorder. This regression may involve language, social skills, motor skills, and self-help skills. The speed and extent of regression can differ among children.
It's important to note that while some children may experience a plateau or stabilization of symptoms, many continue to face ongoing challenges throughout their lives. The long-term prognosis for children with CDD is generally guarded, and they may require ongoing support and intervention to manage their symptoms and improve their quality of life.
Long-Term Considerations and Support Options
When it comes to managing CDD in the long term, a multidisciplinary approach is crucial. This involves a team of healthcare professionals, educators, therapists, and caregivers working together to provide comprehensive support and intervention.
Some long-term considerations and support options for children with CDD include:
Education and Individualized Learning
Children with CDD often require specialized education and individualized learning plans to address their unique needs and challenges. Special education programs that focus on communication, social skills development, and adaptive learning strategies can play a vital role in helping children with CDD reach their full potential.
Behavioral and Communication Interventions
Behavioral and communication interventions are essential components of managing CDD. Applied Behavior Analysis (ABA) therapy and speech-language therapy can help children with CDD develop functional communication skills, manage challenging behaviors, and improve their social interactions.
Occupational and Physical Therapy
Occupational and physical therapy can assist children with CDD in enhancing their motor skills, coordination, sensory processing, and self-care abilities. These therapies focus on improving independence and overall functioning in daily activities.
Supportive Services and Community Resources
Access to supportive services and community resources is vital for families of children with CDD. Support groups, respite care, counseling services, and community organizations can provide valuable emotional support, information, and resources to help families navigate the challenges associated with CDD.
It's important for families to work closely with healthcare professionals to develop an individualized treatment plan that addresses the specific needs of the child. While the long-term outlook for children with CDD can be challenging, early intervention and ongoing support can make a significant difference in their overall well-being and quality of life.
Resources and Further Information
When it comes to childhood disintegrative disorder (CDD), it's important to have access to reliable resources and support networks. Here are some organizations and support groups that can provide valuable information and assistance to individuals and families dealing with CDD.
Organizations and Support Groups
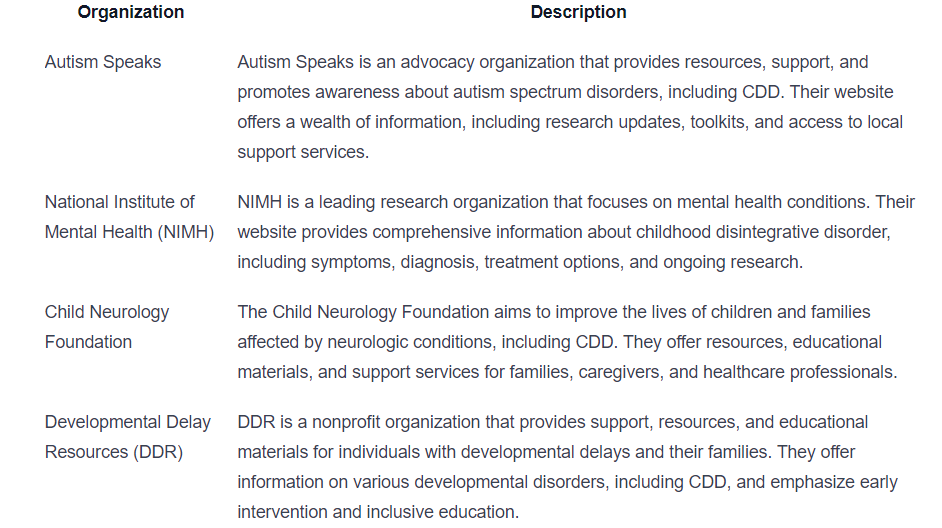
Additional Reading and References
In addition to organizations and support groups, there are several books, articles, and research papers that provide further insights into childhood disintegrative disorder. Here are some recommended readings and references for those seeking more in-depth information:

These resources can provide a deeper understanding of CDD, its symptoms, diagnostic criteria, treatment approaches, and long-term considerations. It is always recommended to consult with healthcare professionals and specialists for personalized advice and guidance based on individual circumstances.
Remember, knowledge and support are essential in managing childhood disintegrative disorder. By utilizing these resources, individuals and families can access valuable information, connect with others facing similar challenges, and explore various strategies to support their loved ones with CDD.
Sources
https://www.mountsinai.org/health-library/diseases-conditions/childhood-disintegrative-disorder
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3401658/
https://emedicine.medscape.com/article/916515-overview
Similar articles
We’re here to help you

Our team is here to assist you in this process. Contact us for any assistance.
it’s easy to apply
We Accept Most Insurances
Our in-network insurance partnerships make ABA therapy more accessible to families throughout our service areas.







Our Insurance Process
We'll request your insurance details to help us verify your plan's coverage for ABA therapy. Once we've received this information, we'll walk you through your benefits, including copayments, deductibles and out-of-pocket maximums, so you know what to expect in advance.
Our team will then handle the preauthorization and all the necessary paperwork.
.svg)


















.jpeg)


























.jpeg)




.jpeg)







.jpeg)










.jpeg)