Autism and Bed Wetting: The Surprising Connection
Unveiling the hidden link between autism and bedwetting. Explore the surprising connection and strategies for support.

Understanding Autism and Bedwetting
To comprehend the surprising connection between autism and bedwetting, it is important to first gain an understanding of autism spectrum disorder (ASD) and explore the occurrence of bedwetting in children with autism.

Overview of Autism Spectrum Disorder (ASD)
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that affects communication, social interaction, and behavior. It is characterized by a wide range of symptoms and varying degrees of impairment. Children with ASD may have difficulties with verbal and nonverbal communication, social interactions, repetitive behaviors, and sensory sensitivities.
ASD is diagnosed based on the presence of certain behavioral criteria according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). It is important to note that while bedwetting is not a diagnostic criterion for ASD, there is evidence of a higher prevalence of bedwetting among children with ASD compared to their typically developing peers.
Exploring Bedwetting in Children with Autism
Bedwetting, also known as nocturnal enuresis, refers to the unintentional release of urine during sleep in children over the age of five. While bedwetting is a common issue among young children, the prevalence is higher in children with ASD.
Research suggests that the rate of bedwetting in children with ASD is approximately 30-60%, compared to around 15% in the general population. The reasons for this elevated prevalence are still being investigated, and several factors may contribute to the connection between autism and bedwetting.
Prevalence of Bedwetting
Children with ASD: 30-60%
General Population: Around 15%
The exact mechanisms underlying the link between autism and bedwetting are not fully understood. However, some potential factors that may contribute to bedwetting in children with ASD include:
- Sensory processing issues: Children with ASD often have sensory sensitivities, and these sensitivities may extend to bladder sensations, leading to difficulties in recognizing and responding to the need to urinate.
- Sleep disturbances: Sleep problems are common in children with ASD, and disrupted sleep patterns may contribute to bedwetting.
- Developmental delays: Children with ASD may experience delays in achieving nighttime bladder control, leading to a higher incidence of bedwetting.
Understanding the connection between autism and bedwetting is crucial for developing effective strategies to address this issue in children with ASD. By recognizing the challenges faced by parents and caregivers and implementing appropriate management techniques, it is possible to support children with autism and reduce the impact of bedwetting on their daily lives.
The Surprising Connection
Research has uncovered a surprising connection between autism and bedwetting, shedding light on the overlap between these two seemingly unrelated conditions. Let's delve into the research findings and explore possible explanations for this intriguing link.
Research Findings on Autism and Bedwetting
Multiple studies have shown a higher prevalence of bedwetting, also known as nocturnal enuresis, among children with autism spectrum disorder (ASD) compared to their neurotypical peers. These findings highlight the need for further investigation into the relationship between these two conditions.
A study published in the Journal of Autism and Developmental Disorders examined the prevalence of bedwetting in children with ASD. The researchers found that approximately 30% of children with ASD experience bedwetting, which is significantly higher than the general population where the prevalence ranges from 5% to 10%.
Another study published in the Journal of Pediatric Urology analyzed the characteristics of bedwetting in children with ASD. The researchers discovered that children with ASD who wet the bed tended to have more severe symptoms compared to those without ASD. This suggests a potential association between the severity of autism symptoms and the occurrence of bedwetting.
Possible Explanations for the Link
While the exact mechanisms underlying the connection between autism and bedwetting remain unclear, several theories have been proposed to explain this intriguing link.
One theory is that both conditions share common underlying factors, such as developmental delays or abnormalities in the central nervous system. These shared factors could contribute to difficulties in bladder control and sensory processing, leading to bedwetting in children with autism.
Additionally, sleep disturbances are common in individuals with ASD. It is possible that disruptions in sleep patterns, such as fragmented sleep or altered sleep architecture, may contribute to bedwetting episodes. Sleep abnormalities can affect the functioning of the bladder and may be a contributing factor to bedwetting in children with autism.
Furthermore, the presence of comorbid conditions, such as attention deficit hyperactivity disorder (ADHD) or anxiety, which are more prevalent in individuals with ASD, may also influence the occurrence of bedwetting. These conditions can impact bladder control and contribute to bedwetting episodes.
While more research is needed to fully understand the complex relationship between autism and bedwetting, these theories provide valuable insights into the potential mechanisms at play.
By further exploring the research findings and investigating possible explanations, we can gain a deeper understanding of the surprising connection between autism and bedwetting. This knowledge can help inform strategies for managing bedwetting in children with autism and improve the overall care and support provided to individuals with these overlapping conditions.
Addressing Bedwetting in Children with Autism
Parents and caregivers of children with autism often face unique challenges when it comes to addressing bedwetting. It's important to understand these challenges and implement strategies that can help manage this issue effectively.
Challenges Faced by Parents and Caregivers
Bedwetting, also known as nocturnal enuresis, can be particularly challenging for children with autism. Some of the difficulties faced by parents and caregivers include:
- Communication barriers: Children with autism may have difficulty expressing their needs and sensations, making it challenging for them to communicate about their bedwetting episodes.
- Sensory issues: Sensory sensitivities commonly associated with autism may contribute to bedwetting. Children may have difficulty recognizing the sensation of a full bladder or may not wake up when they need to go to the bathroom.
- Sleep disturbances: Sleep problems are prevalent in children with autism, and bedwetting can further disrupt their sleep patterns, leading to additional challenges for both the child and caregiver.
- Emotional impact: Bedwetting can affect a child's self-esteem and cause emotional distress. It's essential for parents and caregivers to provide support and understanding to help the child cope with these feelings.
Understanding these challenges is the first step toward finding effective solutions for managing bedwetting in children with autism.
Strategies for Managing Bedwetting
While there is no one-size-fits-all approach to managing bedwetting in children with autism, several strategies can be helpful:
- Establish a routine: Implementing a consistent bedtime routine can help regulate the child's sleep patterns and create a conducive environment for better bladder control.
- Encourage regular bathroom breaks: Remind the child to use the bathroom before bedtime and during the day at regular intervals. Setting timers or using visual schedules can assist in establishing a routine.
- Limit fluid intake before bedtime: Encourage the child to drink fluids earlier in the day and reduce intake closer to bedtime to minimize the likelihood of bedwetting.
- Use protective bedding: Utilize waterproof mattress covers and protective bedding to make cleanup easier and reduce the impact of bedwetting on the child's sleep environment.
- Positive reinforcement: Provide praise and rewards for dry nights to motivate the child and reinforce positive behavior.
- Consult a healthcare professional: It's important to involve healthcare providers experienced in autism and bedwetting to assess the underlying causes and discuss potential interventions or treatments.
It's vital for parents and caregivers to approach bedwetting with patience, understanding, and a collaborative mindset. By implementing appropriate strategies and seeking professional guidance, the challenges associated with bedwetting in children with autism can be effectively managed, improving the overall well-being of the child and their caregivers.
Seeking Professional Help
When dealing with bedwetting in children with autism, it is essential to seek professional help to address the issue effectively. Consulting healthcare providers who specialize in autism spectrum disorder (ASD) and pediatric care can provide valuable guidance and support.
Importance of Consulting Healthcare Providers
Consulting healthcare providers is crucial for several reasons. They have the expertise and knowledge to assess the individual needs of children with autism and bedwetting. These professionals can help identify underlying factors contributing to bedwetting, such as sensory issues, communication challenges, or medical conditions. By understanding the unique needs and characteristics of each child, healthcare providers can develop personalized strategies and interventions.
Additionally, healthcare providers can offer emotional support and reassurance to parents and caregivers. They can address concerns, answer questions, and provide guidance on managing bedwetting in the context of autism. Collaborating with healthcare providers allows for a comprehensive approach that considers the physical, emotional, and behavioral aspects of the child's well-being.
Potential Treatments and Interventions
Healthcare providers may recommend various treatments and interventions to manage bedwetting in children with autism. These can include:
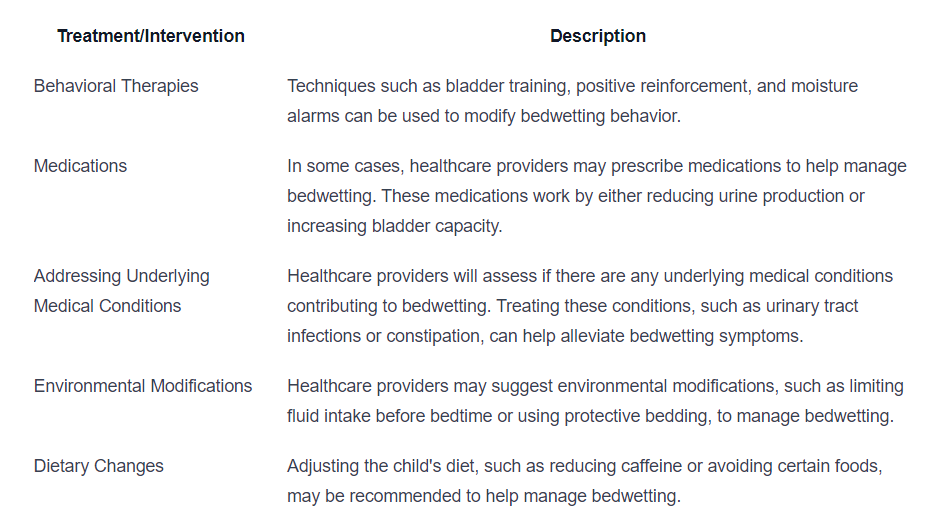
It is important to note that the most appropriate treatment approach may vary depending on the individual needs and circumstances of each child. Healthcare providers will work closely with parents and caregivers to develop a tailored plan that takes into account the child's specific challenges and goals.
By seeking professional help, parents and caregivers can access the expertise and guidance necessary to effectively address bedwetting in children with autism. Collaborating with healthcare providers ensures a comprehensive approach to support the child's well-being, while also providing support and reassurance to the entire family.
Supporting Children with Autism and Bedwetting
When it comes to children with autism who experience bedwetting, providing a supportive and understanding environment is crucial. Here are two key approaches that can help in supporting these children effectively.
Creating a Supportive Environment
Creating a supportive environment involves understanding and addressing the unique needs of children with autism who struggle with bedwetting. Here are some strategies that can contribute to a supportive environment:
- Open Communication: Encourage open and non-judgmental communication with the child. Allow them to express their feelings and concerns regarding bedwetting without fear of criticism or punishment.
- Patience and Understanding: Recognize that bedwetting is a common challenge faced by many children with autism. Approach the situation with empathy, understanding that the child may have limited control over their bladder function.
- Establishing Routine: Establishing a consistent bedtime routine can help children with autism feel more secure and relaxed. A predictable routine can contribute to better sleep patterns, potentially reducing the occurrence of bedwetting incidents.
- Safe and Comfortable Sleeping Environment: Ensure that the child's sleeping environment is safe and comfortable. Consider using waterproof mattress covers and protective bedding to minimize the impact of bedwetting incidents.
Encouraging Positive Coping Mechanisms
Encouraging positive coping mechanisms can help children with autism develop effective strategies to manage bedwetting. Here are some approaches that can be beneficial:
- Encourage Toileting Habits: Establish a regular toileting schedule, including before bedtime, to help empty the bladder before sleep. Remind the child to use the bathroom and provide positive reinforcement for successful toileting.
- Reward Systems: Implement a reward system to motivate the child to stay dry throughout the night. This can involve small rewards or incentives for dry nights or progress made in managing bedwetting.
- Bedwetting Alarms: Bedwetting alarms can be effective tools to help children with autism become more aware of their body signals and wake up when they need to use the bathroom. These alarms can alert the child and their caregiver when an accident occurs, allowing for prompt action.
- Visual Cues and Social Stories: Utilize visual cues and social stories to help children with autism understand the importance of dry nights and the steps they can take to achieve them. Visual schedules and reminders can aid in reinforcing positive habits.
By creating a supportive environment and encouraging positive coping mechanisms, parents and caregivers can help children with autism navigate the challenges of bedwetting. It's important to remember that every child is unique, and what works for one may not work for another. Tailor strategies to the specific needs and preferences of the child, and consider seeking guidance from healthcare providers or specialists experienced in autism care.
Looking Towards the Future
As research on the connection between autism and bedwetting continues to expand, promising developments are emerging. These advancements offer hope for improved understanding and care for individuals affected by both conditions.
Promising Developments in Research
Researchers are actively investigating the underlying mechanisms that contribute to the link between autism and bedwetting. Some recent studies have suggested potential factors that may play a role in this connection. For example, abnormalities in the brain's control over bladder function and sleep patterns have been identified as potential contributors.
Ongoing research is also exploring genetic factors that may be involved in both autism and bedwetting. By uncovering the genetic basis of these conditions, scientists hope to gain a better understanding of the shared pathways and identify potential therapeutic targets.
Hope for Improved Understanding and Care
As our understanding of autism and bedwetting deepens, there is growing optimism for improved care and management strategies. By recognizing the unique challenges faced by individuals with autism and bedwetting, healthcare professionals can develop targeted interventions and support systems.
With the development of evidence-based guidelines, parents and caregivers can access comprehensive resources to help manage bedwetting in children with autism. Strategies such as behavioral interventions, bladder training, and medication options can be tailored to meet the specific needs of each individual.
Furthermore, the advancement of assistive technologies and wearable devices holds promise for monitoring and managing bedwetting in children with autism. These innovations may provide valuable insights into patterns and triggers, allowing for more personalized and effective interventions.
By bringing together the expertise of healthcare providers, researchers, and support networks, there is hope for improved understanding and care for individuals affected by both autism and bedwetting. The collaborative efforts of these stakeholders aim to enhance the quality of life for individuals with autism and provide the necessary support for them and their families.
Through ongoing research, advancements in treatment options, and increased awareness, we can strive to create a future where individuals with autism and bedwetting receive the care and support they need to thrive.
Sources
https://www.apexaba.com/blog/autism-and-bed-wetting
https://www.crossrivertherapy.com/autism/bed-wetting
https://www.myteamaba.com/resources/autism-and-bed-wetting
Similar articles
We’re here to help you

Our team is here to assist you in this process. Contact us for any assistance.
it’s easy to apply
We Accept Most Insurances
Our in-network insurance partnerships make ABA therapy more accessible to families throughout our service areas.







Our Insurance Process
We'll request your insurance details to help us verify your plan's coverage for ABA therapy. Once we've received this information, we'll walk you through your benefits, including copayments, deductibles and out-of-pocket maximums, so you know what to expect in advance.
Our team will then handle the preauthorization and all the necessary paperwork.
.svg)


















.jpeg)


























.jpeg)




.jpeg)







.jpeg)










.jpeg)